

A 36-year-old nurse presented with multiple area of itchy skin. She does bedside nursing at one of the community hospitals and also has a part time job working in one of the local psychiatric nursing facilities. She began to notice the onset of itching in her hands and attributed the symptoms to a change in the hand washing soap used in the hospital. In spite of her using a substitute soap, the pruritus remained and began to spread to other areas of the body, including elbows, axillae, and her back. She then assumed the increased symptoms were due to an allergic reaction to something she had been eating. Although she became very careful with her diet and refrained from eating things to which she thought she might be allergic, the symptoms became worse. At that point, she then decided to see her physician.
Positive findings were limited to the skin, with evidence of intense scratching where the skin was excoriated over the hands and arms. There were also some papules seen on her back. Scrapings of some of these lesions revealed the following:
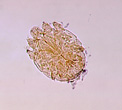
This object measured about 0.25 mm and was almost clear. There were some other structures in the specimen, but they could not be identified.
Scroll Down for Answer and Discussion
Answer and Discussion of Quiz #16
The image presented in Diagnostic Quiz #16 is the following:
Comment: This is a case of a woman who had scabies, caused by the itch mite, Sarcoptes scabiei. She was treated and no new lesions appeared. Although the pruritus continued for several weeks, the use of Calamine lotion reduced the symptoms. With followup, two additional patients on the same ward were also found to have scabies, both of whom responded well to therapy.
In addition to the skin scrapings, the clinical picture was diagnostic. One acquires the infection by close contact. She probably acquired the infection while bathing or caring for the patient; linens and towels can also be involved in transmission. In a situation where an index case is found, other patients with similar symptoms may be treated. The drug of choice is 5% permethrin, applied as a topical cream. A mild steroid cream may also be helpful in sensitive individuals.
|
|
|
Three examples of Sarcoptes scabiei from skin scrapings. The different colors reflect the use of different filters and light microscopy options. It is important to remember that the light should not be too bright; if so, the organisms will appear clear and will not be visible.
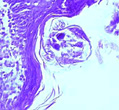
This is a tissue slide of Sarcoptes scabiei, the itch mite.
Usual skin sites are the interdigital spaces, backs of the hands, elbows, axillae, groin, breasts, umbilicus, penis, shoulder blades, small of the back, and buttocks. The outstanding clinical symptom is intense itching. Scratching commonly causes weeping, bleeding, and sometimes secondary infection. A form of the infestation called Norwegian scabies can occur in immunosuppressed or anergic individuals; many mites are present in keratotic excrescences on the body and extremities, but pruritus is usually absent. Such individuals will harbor thousands of mites compared to the normal case with no more than a dozen or two at any given time. Scabies is highly contagious and has been reported as the cause of hospital epidemics. Specific recovery techniques are listed below.
Skin Scraping Technique
Diagnosis can be confirmed by demonstration of the mites, eggs, or scybala (fecal pellets). Because the mites are located under the surface of the skin, scrapings must be made from the infected area.
Plastic Box or Petri Dish Method
If mineral oil preparations of skin scrapings fail to demonstrate the mites, the encrusted skin scrapings, etc., can be placed in a small plastic box or small petri dish. The container should be left undisturbed at room temperature for 12 to 24 h. Away from the living host, the mites will drop down onto the bottom of the box or dish and can be seen with a magnifying glass or with a dissecting microscope.
References:
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.