Quiz 44
Presentation of Quiz #44
Approximately 8 days after attending a wedding banquet, a number of the guests had complained of intestinal symptoms. After carefully assessing symptoms and event-related exposure information from all those who attended the banquet, and examining a minimum of one stool specimen from the guests, it appeared that the illness was probably associated with the ingestion of the wedding cake. Between each cake layer was a layer of filling sauce prepared from fresh raspberries and strawberries.
Each case was defined as onset of the symptoms from 1-14 days after the banquet and either:
- One positive stool specimen and a minimum of one gastrointestinal (GI) symptom (diarrhea, nausea, vomiting, stomach cramps, gas or bloating, loss of appetite, and weight loss) or other symptom (fever, chills, muscle aches, generalized body aches, and headaches), or
- Any diarrhea in a 24-h period and at least one other GI or other symptom, or
- A total of at least 3 GI symptoms.
Laboratory results revealed the following:
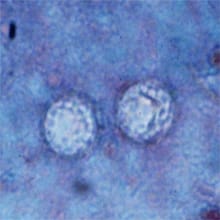
These two structures on the trichrome permanent stained slide failed to stain and measured approximately 9 microns in diameter. They appeared to be somewhat "wrinkled" with no internal structure. A number of these structures were seen on the smear. |
Scroll Down for Answer and Discussion
Answer and Discussion of Quiz #44
The image presented in Diagnostic Quiz #44 is the following:
- This image contains Cyclospora cayetanensis oocysts; these oocysts measure approximately 8 to 10 microns and will not stain with the routine trichrome stain. Based on the structures seen in the routine trichrome stained slides, additional slides were prepared from concentrated stool sediment (500 Xg for 10 min) and stained using the modified acid-fast stain.
Comment:
There is generally 1 day of malaise and low-grade fever, with rapid onset of diarrhea of up to seven stools per day. There may also be fatigue, anorexia, vomiting, myalgia, and weight loss with remission of self-limiting diarrhea in 3 to 4 days, followed by relapses lasting from 4 to 7 weeks. In patients with AIDS, symptoms may persist for as long as 12 weeks; biliary disease has also been reported in this group. Diarrhea alternating with constipation has also been reported; this is not uncommon in a number of protozoal gastrointestinal infections. The majority of infected individuals have intermittent diarrhea for 2 to 3 weeks, and many complained of intense fatigue, as well as anorexia and myalgia, during the illness. The clinical presentation of patients infected with this organism is similar to that of patients infected with Cryptosporidium spp.
Outbreaks in the United States and Canada during the spring months of 1996 and 1997 were related to the importation and ingestion of Guatemalan raspberries. It is quite likely that the outbreak reported from Florida in 1995 was also attributed to contaminated food. Cases reported in all three outbreaks probably represented only a small fraction of those that occurred. The transmission of Cyclospora is thought to be fecal-oral, although direct person-to-person transmission has not be well documented and may not be a factor since sporulation takes a number of days. Outbreaks linked to contaminated water and various types of fresh produce (raspberries, basil, baby lettuce leaves, and snow peas) have been reported.
Life Cycle:
Unsporulated oocysts are passed in the stool and sporulation occurs within approximately 5 to 13 days. In patients who are found to have Cyclospora in their stool specimens, parasites with coccidian characteristics have been found within the jejunal enterocytes. Complete sporulation produces two sporocysts that rupture to reveal two crescent-shaped sporozoites measuring 1.2 by 9.0 μm.
Diagnosis:
In wet mounts, the organisms are seen as nonrefractile spheres and are acid-fast variable with the modified acid-fast stain; those that are unstained appear as glassy, wrinkled spheres. Modified acid-fast stains stain the oocysts from light pink to deep red, some of which will contain granules or have a bubbly appearance. It is very important to be aware of these organisms when the modified acid-fast stain is used for Cryptosporidium spp. and other similar but larger structures (approximately twice the size of Cryptosporidium oocysts) are seen in the stained smear. It is important for laboratories to measure all acid-fast oocysts, particularly if they appear to be somewhat larger than those of Cryptosporidium. The oocysts autofluoresce strong green (450 to 490 DM excitation filter) or intense blue (365 DM excitation filter) under UV epifluorescence. It is strongly recommended that during concentration (formalin/ethyl-acetate) of stool specimens, the centrifugation time and speed should be 10 minutes at 500 x g.
Using a modified safranin technique, the oocysts uniformly stain a brilliant reddish orange if fecal smears are heated in a microwave during staining. The stained slide can also be examined using epifluorescence microscopy first, and suspect oocysts can be confirmed using brightfield microscopy.
Epidemiology and Control:
Published reports indicate that individuals of all ages, including those who are immunocompetent and immunosuppressed, can become infected. In Peru, infections with Cyclospora have shown some seasonal variation, with peaks during the April-to-June time frame. This pattern is similar to that seen in Peru in Cryptosporidium infections. Preliminary data and extrapolation from what we currently know about cryptosporidiosis suggest that modes of transmission may be similar, particularly considering waterborne transmission. Certainly it is recommended that fresh produce be thoroughly washed prior to ingestion.
Cyclospora cayetanensis Key Points–Laboratory Diagnosis
- Specimens may appear as larger than normal Cryptosporidium oocysts; be sure to measure these organisms to confirm size.
- Fecal specimens should be concentrated prior to staining; centrifugation for 10 minutes at 500 xg is recommended.
- On wet smears, the oocysts will appear as nonrefractile spheres and will autofluoresce from bright green to intense blue with epifluorescence.
- On modified acid-stained smears, the oocysts will stain from light pink to deep red, some of which will contain granules or have a bubbly appearance.
Those that do not stain may have a wrinkled appearance. Remember: do not use a strong decolorizer; a 1% sulfuric acid is recommended and will also work well for modified acid-fast stains for Cryptosporidium spp. and/or Cystoisospora belli. The original 3-5% sulfuric acid is usually too strong for Cyclospora and removes too much color. Even with the 1% acid decolorizer, some oocysts may appear clear or very pale. 5. If they are seen in a regular trichrome-stained smear of stool, the oocysts may appear as clear, round, somewhat wrinkled objects that measure larger than Cryptosporidium. 6. It is very important to measure these oocysts; Cyclospora oocysts measure from 8 to 10 microns, and Cryptosporidium oocysts measure from 4 to 6 microns.
Treatment: Trimethroprim-sulfamethoxazole (TMP-SMX) is currently the drug of choice; relief of symptoms has been seen in 1 to 3 days posttreatment. However, recurrence of symptoms can occur within 1 to 3 months posttreatment in over 40% of the patients. In a study using TMP-SMX in Nepal, shedding of oocysts and symptoms disappeared after 7 days of treatment.
|
||
Three images of Cyclospora cayetanensis oocysts from a positive stool specimen (from left to right: autofluorescence using Calcofluor filters; modified acid-fast stain; modified acid-fast stain showing Cyclospora [large], Cryptosporidium [medium], and a pink artifact [small]). Note the oocysts in the modified acid-fast stain range from clear to dark pink to red or even purple. The oocysts are often described as looking like "wrinkled cellophane" and measure 8 to 10 microns. Cryptosporidiumoocysts measure 4 to 6 microns. |
||
References:
- Garcia, LS, 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, DC.
- Garcia, L.S. 2009. Practical Guide to Diagnostic Parasitology, 2nd Ed., ASM Press, Washington, D.C.
Quizzes
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.
- Quiz 1
- Quiz 2
- Quiz 3
- Quiz 4
- Quiz 5
- Quiz 6
- Quiz 7
- Quiz 8
- Quiz 9
- Quiz 10
- Quiz 11
- Quiz 12
- Quiz 13
- Quiz 14
- Quiz 15
- Quiz 16
- Quiz 17
- Quiz 18
- Quiz 19
- Quiz 20
- Quiz 21
- Quiz 22
- Quiz 23
- Quiz 24
- Quiz 25
- Quiz 26
- Quiz 27
- Quiz 28
- Quiz 29
- Quiz 30
- Quiz 31
- Quiz 32
- Quiz 33
- Quiz 34
- Quiz 35
- Quiz 36
- Quiz 37
- Quiz 38
- Quiz 39
- Quiz 40
- Quiz 41
- Quiz 42
- Quiz 43
- Quiz 44
- Quiz 45
- Quiz 46
- Quiz 47
- Quiz 48
- Quiz 49
- Quiz 50
- Quiz 51
- Quiz 52
- Quiz 53
- Quiz 54
- Quiz 55
- Quiz 56
- Quiz 57
- Quiz 58
- Quiz 59
- Quiz 60
- Quiz 61
- Quiz 62
- Quiz 63
- Quiz 64
- Quiz 65
- Quiz 66
- Quiz 67
- Quiz 68
- Quiz 69
- Quiz 70
- Quiz 71
- Quiz 72
- Quiz 73
- Quiz 74
- Quiz 75
- Quiz 76
- Quiz 77
- Quiz 78
- Quiz 79
- Quiz 80
- Quiz 81
- Quiz 82
- Quiz 83
- Quiz 84
- Quiz 85
- Quiz 86
- Quiz 87
- Quiz 88
- Quiz 89