

***Reminder: Slides and examination questions are copyrighted and cannot be copied for publication.
1. The correct match between the organism and one method of acquiring the infection is:
a. Trypanosoma brucei rhodesiense - bite of infected sand fleas
b. Plasmodium falciparum – bite of infected triatomid bug
c. Leishmania spp. - skin penetration of infective form from soil
d. Plasmodium vivax – bite of infected female Anopheline mosquito
ANSWER (d): All four species of Plasmodium can be transmitted by the bite of Anopheline mosquitoes.
East and West African trypanosomiasis (Trypanosoma brucei rhodesiense and T. b. gambiense) are acquired when infective forms are introduced into the human body through the bite of the Tsetse fly, not sand fleas. Leishmania spp. are generally transmitted by the bite of various genera of sand flies.
2. Babesia is an organism which has been implicated in disease from both splenectomized and non-splenectomized patients. Morphologically, the parasites resemble:
a. Plasmodium falciparum rings
b. Leishmania donovani amastigotes
c. Trypanosoma cruzi trypomastigotes
d. Plasmodium vivax schizonts
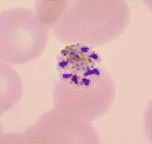
ANSWER (a): Babesia is an intracellular parasite that closely resembles the ring forms (early trophozoites) of Plasmodium falciparum. Often in babesiosis there are more rings per cell and the ring form is the only stage seen. Although the Maltese Cross ring formation is seen in some Babesia spp., it is not evident in all.
3. Which microfilariae are usually not found circulating in the peripheral blood?
a. Brugia malayi
b. Wuchereria bancrofti
c. Onchocerca volvulus
d. Loa loa
ANSWER (c): The microfilariae of Onchocerca volvulus are normally found in the fluid right under the outer layer of skin. Therefore, the skin snip is the proper specimen to examine. The other microfilariae listed can be found in the circulating blood.
4. Massive hemolysis, Blackwater fever and central nervous system involvement are most common with:
a. Plasmodium vivax
b. Plasmodium falciparum
c. Plasmodium ovale
d. Plasmodium malariae
ANSWER (b): The pathogenic sequelae of malarial infections with Plasmodium falciparum are the most severe of the four species and can include massive hemolysis, Blackwater fever and multiple organ involvement, including the central nervous system (cerebral malaria).
5. There are few procedures considered STAT in parasitology. The most obvious situation would be:
a. ova and parasite examination for giardiasis
b. Baermann concentration for strongyloidiasis
c. blood films for malaria
d. culture for amebic keratitis
ANSWER (c): The request for blood films for malaria should always be considered a STAT request. Any laboratory providing these services should have testing available 24 hours per day, 7 days a week. In cases of Plasmodium falciparum malaria, any delay in diagnosing the infection could be fatal for the patient.
6. A 60 year-old Brazilian with cardiac irregularities and congestive heart failure suddenly dies. Examination of the myocardium revealed numerous amastigotes, an indication that the cause of death was probably:
a. leishmaniasis caused by Leishmania donovani.
b. leishmaniasis caused by Leishmania braziliensis.
c. trypanosomiasis caused by Trypanosoma gambiense.
d. trypanosomiasis caused by Trypanosoma cruzi.
ANSWER (d): Trypanosoma cruzi, the cause of Chagas’ disease, has two forms within the human, the trypomastigote in the blood and the amastigote in the striated muscle (cardiac muscle and intestinal tract muscle).
a. diet, age, sex
b. age, antimalarial medication, sex
c. travel history, antimalarial medication, date of return to U.S.
d. fever patterns, travel history, diet
ANSWER (c): Travel history (areas of drug resistance), the date of return to the United States (primary vs. relapse case), and history of antimalarial medication (severe illness, few organisms on smear) are very important questions to ask. Without this information, a malaria diagnosis can be missed or delayed with severe patient consequences.
8. Which of the following is true about onchocerciasis?
a. The adult worm is present in the blood.
b. The microfilariae are in the blood during the late evening hours.
c. The diagnostic test of choice is the skin snip.
d. The parasite resides in the deep lymphatics.
ANSWER (c): The adult Onchocerca volvulus reside in subcutaneous nodules and the microfilariae are found in the fluids right under the outer layers of skin; thus the appropriate diagnostic test is the microscopic examination of skin snips for the presence of microfilariae rather than blood collection.
9. Plasmodium vivax and Plasmodium ovale are similar because they:
a. exhibit Schüffner’s dots and have a true relapse in the life cycle.
b. have no malarial pigment but do have multiple rings per RBC.
c. commonly have appliqué forms in the red cells.
d. have true stippling, do not have a relapse stage, and infect old red cells.
ANSWER (a): Both Plasmodium vivax and Plasmodium ovale infect young red cells, have true stippling (Schüffner’s dots), contain malarial pigment, have a true relapse stage in the life cycle and tend not to have multiple rings per cell.
10. The main differences between finger stick and venipuncture blood are:
a. oxygen content and number of RBCs
b. volume of blood and Plasmodium spp. parasites do not continue developing in finger stick blood
c. parasitemia visible and number of ring forms
d. presence of gametocytes and mature schizonts
ANSWER (b): Usually the amount of blood taken during a finger stick is quite small, while venipuncture blood is often approximately 7ml. Also, when finger stick blood is spread onto the glass slide, the Plasmodium spp. life cycle is stopped at that point, while the life cycle continues in venipuncture blood that remains in the tube prior to blood film preparation.
11. The main benefit of the thin blood film is:
a. RBC morphology is preserved
b. more blood is visible than on the thick blood film
c. the sensitivity is greater than on the thick blood film
d. the specificity is less than on the thick blood film
ANSWER (a): One of the main benefits of the thin blood film is the preservation of the RBC; thus parasites within the RBCs are visible and can be identified. Less blood is seen on the thin blood film; thus sensitivity is less than the thick blood film (less blood). However, specificity is greater on the thin blood film and it is easier to identify the parasites to the genus/species levels.
12. A traveler who has acquired a Plasmodium spp. infection, but who has never been exposed to malaria before is classified as being:
a. immunologically deficient
b. immunologically immunosuppressed
c. immunologically mature
d. immunologically naïve
ANSWER (d): Travelers who have never been exposed to malaria before, but who acquire the infection are referred to as immunologically naïve. They have no pre-existing antibody and are unprotected. Thus, they can become quite ill early on in the infection, unlike a patient living in the endemic area who has residual antibody and who may become symptomatic later in the course of the infection.
13. The main benefit of the thick blood film is:
a. the volume of blood is larger than the thin blood film
b. the thick blood film is less sensitive in terms of organism detection
c. parasite morphology is superior to that on the thin blood film
d. WBCs are no longer visible
ANSWER (a): The volume of blood is larger than that seen on the thin blood film. Actually, the thick film is more sensitive in terms of organism detection, although parasite morphology is not as good as that seen on the thin blood film. Also, on the thick blood film, parasites, platelets, and WBCs are visible.
a. heparin
b. EDTA
c. no anticoagulant is required
d. doesn’t matter
ANSWER (b): Although heparin (green top) or EDTA (lavender top) can be used, EDTA is recommended as providing better organism morphology, particularly for Plasmodium spp. When blood is collected in EDTA, specimens should be processed immediately after blood collection.
15. What type of QC slides should be used for blood parasite work?
a. positive slides containing malarial parasites
b. positive slides containing any blood parasite
c. slides stained with Giemsa stain only
d. patient slide that you are currently staining
ANSWER (d): Regardless of the stain you are using (Giemsa, Wright, Wright/Giemsa, rapid stains), your QC slide is the actual slide you are staining. This approach to QC is acceptable to CAP, as well. Any parasites present will stain like WBCs, so your QC is built into the system.
16. The infective stage from which the patient acquires malaria from the mosquito vector is:
a. the sporozoite
b. the ookinete
c. the gametocyte
d. the exflagellating male gametocyte
ANSWER (a): When the infected Anopheline mosquito takes a blood meal, it injects infective sporozoites into the wound site, thus initiating the malarial infection in the human.
17. Which of the following parasites has been linked to splenectomized patients and transfusion transmission in the eastern United States?
a. Plasmodium vivax
b. Trypanosoma cruzi
c. Babesia spp.
d. Leishmania spp.
ANSWER (c): Babesia infections have been seen in splenectomized patients (Long Island) and have been documented in transfusion transmission in the eastern United States. However, these cases are not limited to the eastern states.
18. A mature schizont is described as having 8 merozoites arranged around the excess malarial pigment and is seen in an infected RBC that is relatively small in size. The Plasmodium species is most probably which of the following:
a. Plasmodium falciparum
b. Plasmodium vivax
c. Plasmodium ovale
d. Plasmodium malariae
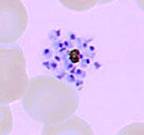
ANSWER (d): The description above refers to the mature schizont of Plasmodium malariae, typically with 8 merozoites arranged like a “daisy head” within small RBCs (older cells).
19. When is the most appropriate time to draw blood for thick and thin blood film preparation for the diagnosis of malaria?
a. when the fever peaks
b. after the fever peaks
c. every 2 hours
d. immediately on request
ANSWER (d): The majority of patients we see in the US with malaria have never been exposed to the organism before; therefore they have no antibody and when they present they do NOT have a synchronized fever cycle. These immunologically naïve patients may present with nonspecific symptoms that can mimic many other diseases. The rule of thumb is to draw immediately; do not wait for some "magic" periodic cycle that may never appear. Patients with a very low parasitemia with P. falciparum can become quite ill before they have any type of fever cycle or gametocytes. With any patient where malaria is suspect or the patient has a FUO (fever of unknown origin), blood should be drawn and both thick and thin blood films prepared and examined immediately. This request is always considered a STAT request.
20. Why is it important that the EDTA blood be processed as quickly as possible, particularly if the cap has been removed and the blood begins to cool down?
a. the WBCs disappear
b. parasite morphology changes occur on standing
c. RBC cell size changes on standing
d. platelets begin to look like malarial ring forms
ANSWER (b): If a tube of blood containing EDTA cools to room temperature and the cap has been removed, several parasite morphologic changes can occur. The parasites within the RBCs will respond as if they were now in the mosquito after being taken in with a blood meal. The morphology of these changes in the life cycle and within the RBCs can cause confusion when examining blood films prepared from this blood. Also after 4-6 hours, parasites begin to disappear from the blood specimen.
A. Stippling (Schüffner’s dots) may not be visible.
B. The male gametocyte (if present) may exflagellate.
C. The ookinetes of Plasmodium species other than P. falciparum may develop as if they were in the mosquito and may mimic the crescent-shaped gametocytes of P. falciparum.
21. New glass slides need to be precleaned prior to blood film preparation because:
a. the blood will fall off both thick and thin blood films
b. no feather edge will be visible
c. holes will be visible in the blood
d. the blood films will not stain
ANSWER (c): Even new slides will be coated with a very fine layer of oil (to allow the slides to be “pulled apart” one from the other) - by removing the coating, the blood will flow more smoothly over the glass during blood film preparation. “Holes” in the blood film are evidence of oil or grease on the slide.
22. Acceptable stain options for blood parasite work include which of the following:
a. Giemsa stain
b. Giemsa, Wright, Wright-Giemsa, Field’s stains
c. Delafield’s hematoxylin stain, rapid blood stains
d. All of the above
ANSWER (d): Although for many years, Giemsa stain has been the stain of choice, the parasites can also be seen on blood films stained with Wright's stain, a Wright/Giemsa combination stain or one of the more rapid stains such as Diff-Quik (American Scientific Products, McGraw Park, IL), Wright’s Dip Stat Stain (Medical Chemical Corp., Torrance, CA), or Field’s stain. It is more appropriate to use a stain with which you are familiar, rather than Giemsa which is somewhat more complicated to use. PMNs will serve as the QC organism for any of the blood stains. Any parasites present will stain like the PMNs, regardless of the stain used. Also, the CAP checklist does not mandate the use of Giemsa stain. Delafield’s hematoxylin is often used to stain the sheath of Wuchereria bancrofti (will not stain using Giemsa stain).
23. How should malaria blood films (both thick and thin films) be examined?
a. 10 min each using 100x oil immersion objective
b. 300 oil immersion fields (using 100x oil objective)
c. 10 min thin, 20 min thick films using 60x oil immersion objective
d. screen using 60x oil immersion objective, 5 min using 100x oil immersion objective
ANSWER (b): A minimum of 300 oil immersion fields using the 100X objective should be examined (for each of the blood films, thick and thin). The blood film can be scanned using a 50X or 60X oil immersion lens, but final reporting of the results should be based on the use of the 100X oil immersion lens for a total magnification of X1,000. “Minutes screened” is normally not used since different individuals screen at different rates. Remember that the entire blood film should be screened using the 10X low power objective to detect microfilariae before moving to oil immersion.
24. It is important to “rule out” infections with Plasmodium falciparum because:
a. this species causes the most serious malarial illness
b. this species is the most common seen in the United States
c. this species infects only the young RBCs
d. this species always causes blackwater fever
ANSWER (a): P. falciparum causes more serious disease than the other three species (P. vivax, P. ovale, and P. malariae). P. falciparum tends to invade all ages of RBCs, and the proportion of infected cells may exceed 50%. Schizogony occurs in the internal organs (spleen, liver, bone marrow, etc.) rather than in the circulating blood. Ischemia caused by the plugging of vessels within these organs by masses of parasitized RBCs will produce various symptoms, depending on the organ involved. However, blackwater fever does not always occur in cases with P. falciparum.
Onset of a P. falciparum malaria attack occurs from 8 to 12 days after infection and is preceded by 3 to 4 days of vague symptoms such as aches, pains, headache, fatigue, anorexia, or nausea. The onset is characterized by fever, a more severe headache, and nausea and vomiting, with occasional severe epigastric pain. There may be only a feeling of chilliness at the onset of fever. Periodicity of the cycle will not be established during the early stages, and the presumptive diagnosis may be totally unrelated to a possible malaria infection. If the fever does develop a synchronous cycle, it is usually a cycle of somewhat less than 48 h. An untreated primary attack of P. falciparum malaria usually ends within 2 to 3 weeks. True relapses from the liver do not occur, and after a year, recrudescences are rare. Severe or fatal complications of P. falciparum malaria can occur at any time during the infection and are related to the plugging of vessels in the internal organs, the symptoms depending on the organ(s) involved. NOTE: The primary objective when performing blood film examination for parasites is to “rule out P. falciparum.” Although rare, it is now important to examine the blood films for the possibility of infection with the fifth human malaria, P. knowlesi (can cause severe disease).
25. RBCs containing multiple rings/cell are usually seen in infections with:
a. Plasmodium vivax
b. Plasmodium ovale
c. Plasmodium malariae
d. Plasmodium falciparum
ANSWER (d): Although multiple rings/cell are occasionally seen in infections with P. vivax, examples are much more common in infections with P. falciparum.
26. A mature schizont containing 16-18 merozoites within an enlarged RBC is most likely:
a. Plasmodium falciparum
b. Plasmodium vivax
c. Plasmodium ovale
d. Plasmodium malariae
ANSWER (b): Both P. vivax and P. ovale tend to infect young RBCs that appear to be enlarged. However, the mature schizont of P. vivax contains approximately 16-18 merozoites.
27. It is important to identify malaria parasites to the species level because:
a. different therapy may be required
b. it is important to anticipate periodicity
c. mixed infections are very common
d. none of the above
ANSWER (a): Since P. falciparum can cause severe disease and death, it is very important for the physician to know whether this infection can be “ruled out.” It is also important to know if any of the other three species are present, particularly P. vivax or P. ovale, which would require therapy for both the liver and RBC stages due to potential relapse from the liver stages. It is also important because of potential drug resistance [chloroquine, P. falciparum, P. vivax; primaquine tolerance/resistance, P. vivax (rare, but documented)].
28: Finding only ring forms on two sets of blood films drawn 6 h apart may suggest:
a. the possibility of a mixed infection
b. the possibility of an infection with P. vivax
c. the probability of an infection with P. falciparum
d. the probability of an infection with P. ovale
ANSWER (c): Remember that all of the life cycle stages (rings, developing trophozoites, early schizonts, late schizonts, mature schizonts, and gametocytes) can be seen on the blood films in infections with P. vivax, P. ovale, and P. malariae. Due to unique characteristics of the life cycle, only rings and gametocytes (and occasional mature schizonts) are seen in the peripheral blood with a P. falciparum infection. Therefore, if you see two sets of blood films (collected 6 h apart) that contain ring forms only, there is an excellent chance the patient is infected with P. falciparum, the most serious of the four Plasmodium spp. infections.
29. Infections with P. ovale or P. vivax rarely go above:
a. 20%
b. 10%
c. 7%
d. 2%
ANSWER (d): Because they infect young RBCs only, the parasitemia rarely goes above 2%.
30. Why aren’t gametocytes of P. falciparum seen in many patients presenting to the Emergency Room (ER)?
a. no gametocytes are formed in most infections
b. it is too early in the cycle to see gametocytes
c. treatment has destroyed the gametocytes
d. the parasitemia is too low
ANSWER (b): Many patients present to the ER early in the infection prior to the formation of the gametocytes; thus the diagnosis must be made based on seeing the ring forms only. As you can imagine, identification of Plasmodium to the species level can be very difficult when rings only are present. These patients tend to be travelers who have had no prior exposure to P. falciparum (immunologically naïve) and who become symptomatic very early after being infected. It normally takes approximately 10 days for the crescent-shaped P. falciparum gametocytes to form.
31. A developing trophozoite has been described as follows: enlarged RBC, very ameboid troph, presence of Schüffner’s dots. The species is most likely:
a. Plasmodium vivax
b. Plasmodium ovale
c. Plasmodium malariae
d. Plasmodium falciparum
ANSWER (a): Although both P. vivax and P. ovale are seen in enlarged RBCs and both have Schüffner’s dots, P. vivax has very ameboid trophs, while those of P. ovale are not.
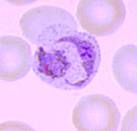
P. vivax P. ovale
32. A trypomastigote seen in a thin blood film is described as being somewhat “C” shaped, has an undulating membrane and a very large kinetoplast. It is most likely:
a. Trypanosoma brucei rhodesiense
b. Trypanosoma rangeli
c. Trypanosoma cruzi
d. Trypanosoma brucei gambiense
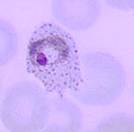
ANSWER (c): Typically, T. cruzi can be seen in a “C” shape, has an undulating membrane like the other trypomastigotes, but has a very large kinetoplast.


T. cruzi T. b. gambiense or rhodesiense
33. The possibility of finding amastigotes in buffy coat cells is limited to:
a. Leishmania tropica
b. Leishmania braziliensis
c. Leishmania donovani
d. All of the above
ANSWER (c): While the amastigotes of L. tropica (cutaneous) and L. braziliensis (mucocutaneous) are found in the macrophages of the skin and mucous membranes, the amastigotes of L. donovani are found in the macrophages of the spleen, liver, bone marrow, and occasionally buffy coat cells (monocytes). Thus, if the lesion is confined to the skin and/or mucous membranes, amastigotes will not be found in the buffy coat cells.
34. Which of the following are important to include in a report from blood film examination for malaria?
a. Genus, species
b. Parasitemia, possible mixed infection
c. Ability to “rule out” P. falciparum
d. All of the above
ANSWER (d): All of the above is the correct response.
Using the thin blood film method, report the percentage of parasite-infected RBCs per 100 RBCs counted.
Example: Plasmodium falciparum, parasitemia = 0.01%
Using the thick/thin blood film method, report the number of parasites per μl of blood.
Example: Plasmodium falciparum, parasitemia = 10,000 per μl of blood
It is important to convey to the physician that P. falciparum cannot be ruled out; therapy may be initiated on the assumption that this species might be present. The report should read:
Example: Plasmodium spp. present; unable to “rule out” Plasmodium falciparum.
It is important to remember that mixed infections are much more common than suspected and/or reported. When rings are present, along with other developing stages (P. vivax, P. ovale, P. malariae) always look for the presence of two populations of ring forms, one of which might be P. falciparum! The report should read:
Example: Plasmodium spp. present, possible mixed infection; unable to “rule out” P. falciparum. Another report example might be: Plasmodium vivax rings, developing schizonts, and gametocytes; possible mixed infection: unable to “rule out” P. falciparum.
35. Proficiency Testing blood films can be examined as follows:
a. Screen with 10x, screen with 60x oil, and 300 fields with 100 x oil objective
b. Screen with 60x oil, 300 fields with 100x oil objective
c. 300 fields with 100x oil objective
d. 100 fields with 100x oil objective
ANSWER (a): Since you have no idea what organisms might be present, always review the blood films using the 10X objective (entire slide). This examination is likely to reveal any microfilariae that are present; however, small parasites like Plasmodium and Babesia may be missed. It is also acceptable to screen the films using a 50 or 60x oil immersion objective; however, remember than very young ring forms can be missed. Therefore, before reporting the smear as negative, examine at least 300 oil immersion fields using the 100X oil immersion lens.
REFERENCES
Garcia, L.S. 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.