

Plasmodium knowlesi (True Pathogen – Monkey Malaria)
Organism:
This organism belongs to the phylum Apicomplexa, is a true pathogen, and causes malaria. All forms of the human life cycle will appear in the thick and thin blood films.
 |
 |
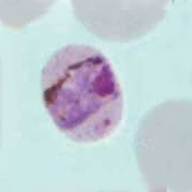 |
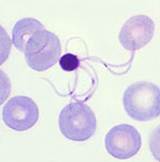
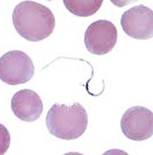
| Plasmodium knowlesi ring forms | P. knowlesi band forms |
As early as 1999, a fifth malaria has been implicated in human disease. Plasmodium knowlesi, a malaria parasite of long-tailed macaque monkeys has been confirmed in a number of human cases from endemic areas such as Malaysian Borneo, Thailand, Myanmar, and the Philippines. Cases have also been found in travelers returning from these areas. Although it is well known that under laboratory conditions some monkey malarias can be transmitted to humans, it is now well established that P. knowlesi is emerging as an important zoonotic human pathogen.
Life Cycle:
Within an hour of infection, sporozoites from the mosquito are carried via the blood to the liver, where they penetrate parenchymal cells, thus initiating the preerythrocytic or primary exoerythrocytic cycle. The sporozoites become round or oval and begin dividing, resulting in large numbers of liver merozoites. P. knowlesi is closely related to P. vivax. However, important differences in P. knowlesi include host blood cell preference (normal size RBCs), absence of a dormant liver stage (the hypnozoite), and length of the asexual cycle (24 h). In P. vivax and P. ovale, a secondary or dormant schizogony occurs from organisms that remain quiescent in the liver until a later time; they are called hypnozoites. Delayed schizogony does not occur in P. falciparum, P. malaria, or P. knowlesi.
P. knowlesi infects all ages of RBCs, and the parasitemia can equal that seen in cases of P. falciparum. Splenomegaly occurs during the first few weeks, and the spleen will progress from being soft and palpable to hard during a chronic infection. If therapy is given early, the spleen will return to normal size. Leukopenia is seen; leukocytosis may be present during the febrile episodes. Total plasma proteins are unchanged, although the albumin may be low and the globulin fraction may be elevated due to antibody development. Serum potassium may also be increased.
Acquired:
Bite: female anopheline mosquito; blood, shared needles, congenital infections
Epidemiology:
Forested areas of Southeast Asia (Malaysian Borneo, Thailand, Myanmar, Philippines).
Clinical Features:
Early Infection: Patients may be asymptomatic, or may exhibit chills, minor headaches and a daily low-grade fever, while other patients may present with high fevers, mild abdominal problems, leukopenia and thrombocytopenia. During the first few days, the patient may not exhibit a typical paroxysm pattern but rather have a steady low‑grade fever or an irregular remittent fever pattern. However, most patients with P. knowlesi malaria have febrile illness and associated symptoms that are indistinguishable from those caused by other malaria species. P. knowlesi requires 24 hours to complete its asexual erythrocytic cycle, which results in a unique quotidian type of fever pattern different from that for the other 4 human malaria species. However, this fever pattern has no practical value for presumptive diagnosis because characteristic fever variations would not be observed during the early phase of infections, and mixed species infections would further complicate pattern recognition related to febrile symptoms.
Complications: Severe complications can be seen in P. knowlesi infections, and coma and sudden death or other symptoms of cerebral involvement have been reported. Autopsy findings are very similar to those seen in fatal P. falciparum malaria, including the cerebral pathology.
Clinical Specimen:
Blood: Multiple draws (EDTA). Malaria is one of the few parasitic infections considered to be immediately life‑threatening, and a patient with the diagnosis of P. falciparum malaria should be considered a medical emergency because the disease can be rapidly fatal. Any laboratory providing the expertise to identify malarial parasites should do so on a 24‑h basis, 7 days/week. Prepare thick and thin blood films immediately after receipt of the blood.
Laboratory Diagnosis:
Although malaria is no longer endemic within the United States, this infection is life threatening, and laboratory requests for blood smear examination and organism identification should be treated as “STAT” requests. Frequently, for a number of different reasons, organism recovery and identification may be more difficult than the textbooks imply. It is very important that this fact be recognized, particularly when one is dealing with a possibly fatal infection with P. falciparum or P. knowlesi. Both thick and thin blood films should be prepared on admission of the patient (clinic, emergency room, in-house), and at least 300 oil immersion fields should be examined on the thick and thin film before a negative report is issued. Since one set of negative films will not rule out malaria, additional blood specimens should be examined over a 36 h time frame. Although Giemsa stain is used for parasitic blood work; the organisms can also be seen with other blood stains such as Wright’s, Wright-Giemsa, or any of the rapid blood stains. Blood collected with EDTA anticoagulant is acceptable; however, if the blood remains in the tube for any length of time, true stippling may not be visible within the infected RBCs (P. vivax as an example), organisms will change their morphology, and some of the parasites will disintegrate (after 4-6 h). Also, it is important to remember that the proper ratio between blood and anticoagulant is necessary for good organism morphology.
NOTE: P. knowlesi infection should be considered in patients with a travel history to forested areas of Southeast Asia, especially if P. malariae is diagnosed, unusual forms are seen with microscopy, or if a mixed infection with P. falciparum/P. malariae is diagnosed. Since the disease is potentially fatal, proper identification to the species level is critical.
Organism Description:
Ring Forms: Ring forms of P. knowlesi tend to mimic those of P. falciparum (headphones, multiple rings/cell, and various sizes of rings). As the rings grow, the infection begins to mimic morphology seen with P. malariae (normal size to small RBCs, band forms, mature schizont like daisy head).
Gametocyte: The gametocytes are round and tend to fill the entire RBC. Exflagellation of the male gametocytes can occur in the blood if the blood cools and becomes aerated (cap removed – lag time between cooling/cap removal and preparation of the thick and thin blood films.
Laboratory Report:
A number of reports can be relevant – remember to add the appropriate report comments.
Report 1: No Parasites Seen: The submission of a single blood specimen will not rule out malaria; submit additional bloods every 4-6 hours for 3 days if malaria remains a consideration.
Report 2: Plasmodium spp. Seen: Unable to rule out Plasmodium falciparum or Plasmodium knowlesi
Report 3: Plasmodium spp., possible mixed infection: Unable to rule out Plasmodium falciparum or Plasmodium knowlesi
Report 4: Negative for parasites using automated hematology instruments. Automated Hematology instruments will not detect low malaria parasitemias seen in immunologically naïve patients (travelers)
Treatment:
Garcia, L.S. 2007. Diagnostic Medical Parasitology, 5th ed., ASM Press, Washington, D.C.
Control:
Improved mosquito control, impregnated bed nets, potential vaccines, prophylaxis
Comments:
It is important to remember that the malarial parasites remain viable in the tube of blood collected using EDTA. If the blood cools and the cap is removed (blood becomes aerated), the organisms then begin the life cycle seen in the mosquito. Thus exflagellation of the male gametocyte can mimic spirochetes when they separate from the gametocyte (see below):
 |
 |
 |