

A 39-year-old female presented with ocular redness and increased eye pain at night, the initial diagnosis was nodular scleritis [Figure upper left]. This patient presented to the emergency department late at night and a nodular mass was recognized under the conjunctiva. When pressure was applied on the nodule, the shape changed as the parasite unfolded (Figure upper right). The entire parasite was removed while alive through an incision in the conjunctiva (Figure lower). She had an eosinophilia of 10%, which dropped to 3% after therapy. This patient had taken an extensive trip to Italy and some other Mediterranean locations.
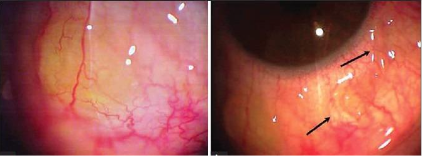
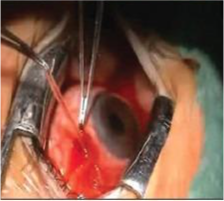
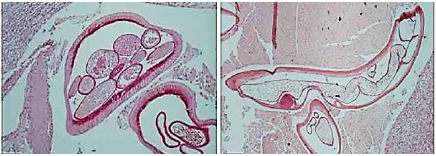
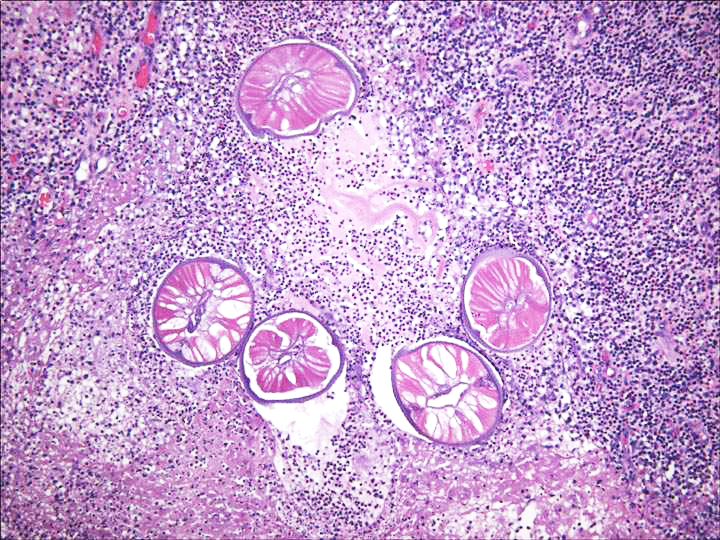
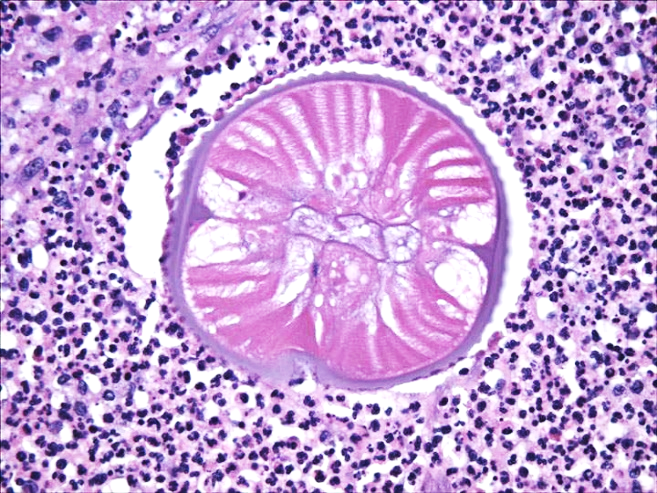
Histopathology revealed cellular infiltration by eosinophils, neutrophils, and granulomatous inflammatory tissue (see image below) (left, PAS, right H&E). Images above and two below courtesy of: Kalogeropoulos CD, Stefaniotou MI, Gorgoli KE, Papadopoulou CV, Pappa CN, Paschidis CA. 2014. Ocular dirofilariasis: a case series of 8 patients. Middle East Afr J Ophthalmol. 21(4):312-6.
What parasitic infections should be considered in the diagnosis?
Do the images shown above provide a diagnosis?
Is her travel history relevant? Why or why not?
Is eosinophilia relevant/helpful?
(Scroll Down for Answers and Discussion)
Based on the images seen above, the presumptive diagnosis would be some type of nematode, perhaps one of the filarial worms such as Dirofilaria (1-5).
Diagnosis can be confirmed by the identification of worms in surgical or autopsy specimens. Because the immature larvae may be detected in only a few microscopic sections, careful histologic examination is necessary.
Ophthalmic infection with Dirofilaria is documented worldwide, including North America, Europe, Australia, Africa, the Middle East, and Asia. Eye involvement may be periorbital, subconjunctival, sub-tenons, or intraocular. Such lesions are usually associated with moderate to severe inflammation. Most cases with eye infections present with pain in the eye, redness, sometimes blurred vision, and swelling of eyelids. Symptoms usually occur weeks or months after infection with microfilaria. Therefore, her travel history is certainly relevant. It is a common zoonosis that rarely infects humans and is considered endemic to Mediterranean countries (Italy, France, Greece, and Croatia). Of the reported cases of human dirofilariasis in Europe, Italy has the highest burden (66% of cases), followed by France (22%), Greece (8%), and Spain (4%).
Peripheral blood eosinophilia and/or presence of eosinophils in affected tissues suggest an allergic reaction caused by the inflammatory response induced by the nematode.
Human dirofilariasis is typically seen as subcutaneous nodules or as lung parenchyma disease. Patients infected with D. repens tend to have a subcutaneous lump (face and conjunctiva of the eye and sometimes chest wall, upper arms, thighs, abdominal wall and male genitalia). Ocular involvement is usually periorbital, orbital, subconjunctival, or sub-tenon infection. Human D. immitis infection is associated with human pulmonary dirofilariasis and is usually asymptomatic. If symptoms are present, they include cough, chest pain, fever, and pleural effusion.
In a very extensive study of over 90 cases of human infection with D. repens, the authors commented on the diagnostic difficulties involved with histologic diagnosis (2). As the worms begin to die within the nodule, the invasion of inflammatory cells begins at the worm’s orifices (mouth, vulva, anus, and cloaca) and gradually spreads throughout its body. It is recommended that the nodule be sectioned at different points in order to review morphologic features that may still be recognizable. This review also contains a series of color photographs in which the nematodes are in an excellent state of preservation, while other photographs illustrate the range of disintegration of the worm within the nodule (Figure 12.3615.34). Dirofilaria are identified by their thick laminated cuticle, broad lateral ends and large muscle cells. D. immitis can be differentiated from D. repens by the absence of ridges
Dirofilaria are identified by their thick laminated cuticle, broad lateral ends and large muscle cells. D. immitis can be differentiated from D. repens by the absence of ridges. Images of D. tenuis below courtesy of Dr. Andrea Linscott.
Although at least 15 species of mosquitoes can carry the infective forms and the infection is considered an emerging zoonosis, probably fewer than 1,000 cases of human infection have been described. However, it is quite possible that many infections go undiagnosed and the number of cases is larger than documented. Canines, cats, foxes, muskrats, otters, and sea lions are natural hosts. The infection in animals has been noted in the United States, Africa, Mediterranean countries, Southeast Asia, and the Pacific Islands. The prevalence of infection in dogs in the southeastern United States may be as high as 40%.
Garcia, L.S, 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.
Pampiglione, S., F. Rivasi, and G. Canestri-Trotti. 1999. Pitfalls and difficulties in histological diagnosis of human dirofilariasis due to Dirofilaria (Nochtiella) repens. Diagn. Microbiol. Infect. Dis. 34:57–64.
Orihel, T. C., and E. K. Isberg. 1990. Dirofilaria striata infection in a North Carolina child. Am. J. Trop. Med. Hyg. 42:124–126.
Simon, F, M Siles-Lucas, R Morchon, J Gonzalez-Miguel, I Mellado, E Carreton, JA Montoya-Alonso. 2012. Human and animal dirofilariasis: the emergence of a zoonotic mosaic. Clin Microbiol Rev 25:507-544.
Marty, AM, RC Neafie. 2000. Dirofilariasis, In: Meyers, WM (ed). Pathology of Infectious Diseases, Vol 1 Helminthiasis, Armed Forces Institute of Pathology, Washington, DC.
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.