

***Reminder: Slides are copyrighted and cannot be copied for publication.
A 27-year-old male with AIDS presented to his physician with a continuing history of symptoms, including chronic intractable diarrhea, fever, malaise, and weight loss. He reported having four to six watery, nonbloody stools per day, and often felt nauseated. The patient had not been taking the highly active antiretroviral therapy (HAART) combination of drugs.
Three ova and parasite examinations had been performed, two of which were reported as negative. The third stool examination revealed the following on the sedimentation concentration wet mount. No organisms were seen on the permanent stained smear (Trichrome).
 |
 |
 |
Please comment on the possible diagnosis related to the history of AIDS, the patient's clinical symptoms and the laboratory test results to date.
(Scroll Down for Answers and Discussions)
ANSWER AND DISCUSSION OF DIAGNOSTIC QUIZ #64
IMAGES:
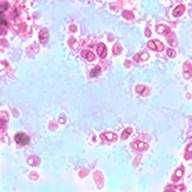
1. Isospora (Cystoisospora) belli oocysts. Note that both oocysts above are immature and contain a single sporocyst. This is typical if the patient has diarrhea. The image on the far right depicts an oocyst containing two mature sporocysts containing sporozoites; this is much more typical if the stool motility is normal (no diarrhea).
ADDITIONAL LABORATORY TEST RESULTS:
Because the patient had AIDS and severe diarrhea, additional tests were requested, including the immunoassay for Cryptosporidium spp. and the modified trichrome stain for microsporidia. The following images were taken from the additional laboratory test results. Note that both the stool and urine were positive for microsporidial spores, probably Encephalitozoon intestinalis or Enterocytozoon bieneusi (or both). The microsporidia are now classified with the fungi.
 |
 |
 |
1. 2. 3.
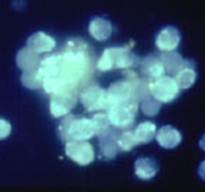
1. Modified trichrome stain (Ryan Blue) - stool
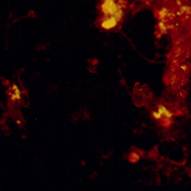
3. Calcofluor white stain – urine
3. Negative FA for Giardia/Cryptosporidium spp. combination reagent
COMMENTS ON THE PATIENT:
This was a case of Isospora belli infection and microsporidiosis in the intestinal tract. The spores seen in the stool and urine measure approximately 1-2 microns, and the morphology does not allow differentiation between the two genera (Enc. intestinalis, Ent. bieneusi). Both can also disseminate to the kidneys and elsewhere, so they could both be found in urine.
Because the patient was not on the HAART regimen, his immune system was less likely to handle infections with Isospora belli, but particularly with microsporidia. Additional images are seen below that demonstrate the use of an experimental FA reagent for the genus Encephalitozoon and a routine tissue section showing the microsporidial spores developing within the intestinal mucosal cells.
1. 2.
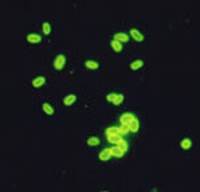
1. Encephalitozoon spp. (probably intestinalis) (Monoclonal reagent)
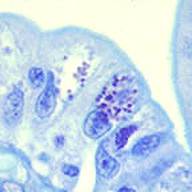
2. Spores in enterocytes (Giemsa stain)
COMMENTS ON DIAGNOSTIC OPTIONS:
Using an experimental monoclonal reagent directed against Encephalitozoon spp., the spores were found to fluoresce, thus confirming spores in this genus were present. Smears were also stained using the optical brightening agent, calcofluor white. Although the spores did stain, this approach is non-specific and results cannot differentiate among the different genera of microsporidia. Unfortunately, commercial immunoassay reagents are not yet available for the detection and/or differentiation of the microsporidia (available in Europe). One can also see the spores within the enterocytes within the intestine; this preparation was stained with Giemsa stain.
Microsporidiosis is an important emerging opportunistic infection in HIV-infected patients and appears to have an ever-expanding clinicopathologic spectrum. This infection has also been identified in transplant patients. Although the majority of information is available regarding the immunocompromised host, it is likely that the immunocompetent host can also acquire these infections; there may be many more infections seen, but not recognized, in normal individuals with diarrhea.
The spore is the only life cycle stage able to survive outside of the host cell and is the infective stage. The spore normally reaches the new host through ingestion, although other routes of infection have been identified including: inhalation, direct inoculation, and sexual transmission. Currently, there are 9 genera and 13 species of microsporidia that have been implicated in human infections. There are a number of methods used for the recovery and identification of microsporidia in clinical specimens. Tissue Gram stains, PAS, silver stains, Giemsa stain or modified trichrome stains are available. Differentiation to the genus level often requires specific experimental reagents or electron microscopy. A positive infection should be reported as: Microsporidian spores seen; unable to identify to the genus level.
KEY POINTS - LABORATORY DIAGNOSIS
1. The modified trichrome staining procedure for stool may be difficult to interpret without positive controls to review (see product information within this web site).
2. Make sure the material on the slides is very thin, the smear is stained for the recommended time frame, and the smear is examined under oil immersion (total magnification of at least x1,000).
3. When using various stains, optical brightening agents, or experimental immunoassay reagents where diagnosis is based on seeing the actual spores, it is highly recommended that the fecal specimen be concentrated and centrifuged at 500 x g for 10 min.
4. The optical brightening agents (calcofluor, FungiFluor, Uvitex 2B) provide a sensitive screening method, but the results are nonspecific. False positives have been reported as a result of fluorescent artifact material.
5. Touch preparations can be methanol fixed and stained with Giemsa.
COMMENTS ON THERAPY:
Although a number of drugs have been tried for microsporidiosis, results have been variable. Agents such as metronidazole, itraconazole, octreotide, primaquine, lomotil, sulfasalazine, loperamide, and albendazole have been used in various patients. In some cases, the diarrhea subsided; however, biopsy specimens showed the continued presence of organisms, which were probably Enterocytozoon bieneusi. Over the past few years, confirmatory evidence indicates that a complete parasitological cure is possible with albendazole. However, these patients had disseminated infections with Encephalitozoon intestinalis; albendazole appears to be very effective in treating this particular organism. Albendazole is a benzimidazole that binds to ß tubulin. Currently, the recommended dose for ocular (Encephalitozoon cuniculi, Vittaforma corneae), intestinal (Enterocytozoon bieneusi, Encephalitozoon intestinalis), and disseminated (Encephalitozoon hellem, E. cuniculi, E. intestinalis, Pleistophora spp., Trachipleistophora spp.) infections with albendazole is 400 mg orally twice a day.
Effective eradication of Isospora belli has been achieved with co-trimoxazole, trimethoprim sulfamethoxazole, pyrimethamine sulfadiazine, primaquine phosphate nitrofurantoin, and primaquine phosphate chloroquine phosphate. Other drugs proven to be ineffective include dithiazanine, tetracycline, metronidazole, phanquone, and quinacrine hydrochloride. The drug of choice is trimethoprim sulfamethoxazole, which is classified as an investigational drug for treatment of this infection. TMP (160 mg) SMX (800 mg) is given every 6 h for 10 days and then twice a day for 3 weeks. In patients allergic to sulfonamides, pyrimethamine alone (50 to 75 mg daily) has cured infections. In immunosuppressed patients with recurrent or persistent infection, therapy must be continued indefinitely.
REFERENCES:
Garcia, LS, 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, DC.
Wittner, M. and L.M. Weiss (eds). 1999. The Microsporidia and Microsporidiosis. ASM Press, Washington, D.C.
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.