

***Reminder: Slides are copyrighted and cannot be copied for publication.
A 23-year old female was first seen in the clinic with complaints of "off and on again" diarrhea and vague symptoms like poor appetite and repeated indigestion. There were two children in the family, a 4-year old male who was in good health and a 2 year-old female who had previously been diagnosed as "failure to thrive." The woman was in good health until about two months prior to becoming symptomatic. She began to have diarrhea with light colored stools, however, this condition was not always present. She complained of lack of appetite, indigestion, and general malaise.
Complete stool examinations were performed (1 O&P exam: direct wet mount, concentration, permanent stained slide and 1 fecal immunoassay for the presumptive diagnosis of giardiasis). All tests had been negative to date.
QUESTIONS
1. Based on the negative laboratory results what would you recommend?
2. Is there a chance that giardiasis could still be the diagnosis? Why or why not?
3. Please comment on the laboratory methods (number and type) performed for this patient? Are you in agreement with the approach? If not, why not; if yes, why?
4. What is meant by “intermittent shedding” – how might this be relevant for this case?
(Scroll Down for Answers and Discussions)
ANSWER AND DISCUSSION OF DIAGNOSTIC QUIZ #60
After repeated O&P examinations and immunoassay testing for Giardia lamblia on two additional fecal specimens, the diagnosis of giardiasis was confirmed. It is not uncommon for the diagnosis of giardiasis to require examination of multiple specimens (O&P, IA testing). It is well known that these organisms are shed on a periodic basis, thus the need for multiple stools for both O&P and immunoassay testing.
 |
 |
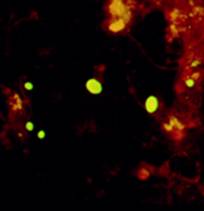 |
The image on the left is a G. lamblia trophozoite from a trichrome-stained permanent stained smear; the organism was seen using the 100X oil immersion objective of the microscope. The organism in the middle shows two G. lamblia cysts stained with iron-hematoxylin stain. Although Giardia lamblia was suspected from the history, the O&P examination and the immunoassay were negative. With the examination of additional specimens, Giardia cysts were seen on the permanent stained smear and the fecal immunoassay was positive. The image on the right is a combination FA test for Giardia lamblia (larger organisms – yellow green) and Cryptosporidium spp.
COMMENTS ON THE ORGANISM:
The incubation time for giardiasis ranges from approximately 12-20 days. Because the acute stage usually lasts only a few days, giardiasis may not be recognized as the cause, but may mimic acute viral enteritis, bacillary dysentery, bacterial or other food poisonings, acute intestinal amebiasis or "traveler's diarrhea" (toxigenic E. coli). However, the type of diarrhea plus the lack of blood, mucus and cellular exudate is consistent with giardiasis. Although the numbers of organisms in the crypts of the duodenal mucosa may reach very high densities, they may not cause any pathology. The organisms feed on the mucous secretions and do not penetrate the mucosa. For some reason, in symptomatic cases, there may be irritation of the mucosal lining, increased mucus secretion, and dehydration.
The acute phase is often followed by a subacute or chronic phase. Symptoms in these patients include recurrent, brief episodes of loose, foul stools; there may be increased distention and foul flatus. Between mushy stools, the patient may have normal stools or may be constipated. Abdominal discomfort continues to include marked distention and belching with a rotten egg taste. Chronic disease must be differentiated from amebiasis and other intestinal parasites such as Dientamoeba fragilis, Cryptosporidium spp., Cyclospora cayetanensis, Isospora belli, and Strongyloides stercoralis and from inflammatory bowel disease and irritable colon. Based on symptoms such as upper intestinal discomfort, heartburn and belching, giardiasis must also be differentiated from duodenal ulcer, hiatal hernia, and gallbladder and pancreatic disease. Because giardiasis may not produce any symptoms at all, demonstration of the organism in symptomatic patients may not rule out other possibilities such as peptic ulcer, celiac disease, strongyloidiasis, and possibly carcinoma.
Giardiasis is one of the more common causes of traveler's' diarrhea and has been recorded from all parts of the world. It has also been speculated that visitors in areas endemic for Giardia are more likely to present with symptoms that those individuals who live in the area; this difference in area residents is most likely due to their development of immunity from prior, and possible continued, exposure to the organism.
LIFE CYCLE:
Both the trophozoite and the cyst are included in the life cycle of G. lamblia. Trophozoites divide by means of longitudinal binary fission, thus producing two daughter trophozoites. The most common location of the organisms is in the crypts within the duodenum. The trophozoites are the intestinal dwelling stage and attach to the epithelium of the host villi by means of the ventral disc. The attachment is substantial and results in disc "impression prints" when the organism detaches from the surface of the epithelium. Trophozoites may remain attached or detach from the mucosal surface. Since the epithelial surface sloughs off the tip of the villus every 72 hours, apparently the trophozoites detach at that time. For reasons which are not totally known, cyst formation takes place as the organisms move down through the colon. The trophozoites retract the flagella into the axonemes, the cytoplasm becomes condensed, and the cyst wall is secreted. As the cyst matures, the internal structures are doubled, so that when excystation occurs the cytoplasm divides, thus producing two trophozoites. Excystation would normally occur in the duodenum.
DIAGNOSIS:
Routine stool examinations are normally recommended for the recovery and identification of intestinal protozoa. However, in the case of G. lamblia, because the organisms are attached so securely to the mucosa by means of the sucking disc, a series of even five or six stools may be examined without recovering the organisms. The organisms also tend to be passed in the stool on a cyclical/periodic basis. The Entero-Test capsule can be helpful in recovering the organisms, as can the duodenal aspirate. Although cysts can often be identified on the wet stool preparation, many infections may be missed without the examination of a permanent stained smear. If material from the string test (Entero-Test) or mucus from a duodenal aspirate is submitted, it should be examined as a wet preparation for motility; however, motility may be represented by nothing more than a slight flutter of the flagella because the organism will be caught up in the mucus. After diagnosis, the rest of the positive material can be preserved as a permanent stain.
Procedures using immunoassays (EIA, FA, cartridge formats) have also been developed to detect Giardia antigen in feces. The immunoassays are more sensitive than the O&P examination. Many of these newer methods are being used to screen patients suspected of having giardiasis or those who may be involved in an outbreak situation. However, it is important to realize that with low numbers of organisms present, even the fecal immunoassays may be negative; it has been recommended that if giardiasis is suspected, two different fecal specimens should be tested using the fecal immunoassay before "ruling giardiasis out" or indicating that infection is much less likely.
STOOL TESTING RECOMMENDED ORDERS
EPIDEMIOLOGY AND CONTROL:
Transmission is by ingestion of viable cysts. Although contaminated food or drink may be the source, intimate contact with an infected individual may also provide the infection mechanism. This organism tends to be found more frequently in children or in groups that live in close quarters. Often there are outbreaks due to poor sanitation facilities or breakdowns as evidenced by travelers and campers. There may also be an increase in the prevalence of giardiasis in the male homosexual population, probably due to anal and/or oral sexual practices. Because of the potential for wild animal reservoir and possibly other domestic animal reservoir hosts, measures in addition to personal hygiene and improved sanitary measures have to be considered. Iodine has been recommended as an effective disinfectant for drinking water, but it must be used according to directions. Filtration systems have also been recommended, although they have certain drawbacks, such as clogging.
Most experts agree that the single most effective practice that prevents the spread of infection in the child care setting is good handwashing by the children, staff, and visitors. Rubbing hands together under running water is the most important part of washing away infectious organisms. Premoistened towelettes or wipes and waterless hand cleaners should not be used as a substitute for washing hands with soap and running water. Certainly these guidelines are not limited to giardiasis, but include all potentially infectious organisms.
GIARDIA LAMBLIA
KEY POINTS--LABORATORY DIAGNOSIS
1. Even if a series of three stool specimens is submitted and examined correctly, the organisms may not be recovered and identified.
2. Motility on wet preparations may be difficult to see because the organisms may be caught up in mucus.
3. Any examination for parasites in stool specimens must include the use of a permanent stained smear (even on formed stool).
4. Duodenal drainage and/or the use of the Entero-Test capsule may be very helpful in organism recovery. However, this technique does not take the place of the ova and parasite examination. The use of immunoassays for antigen detection is now widely used and includes the EIA, FA, and cartridge formats. However, it is important to remember that in a light infection, even the fecal immunoassays may be negative. It is recommended that if the first immunoassay is negative, a second stool should be ordered and retested using the fecal immunoassay.
TREATMENT:
If giardiasis is diagnosed, the patient should be treated. In the majority of cases, metronidazole is the drug of choice, but is still considered investigational. Metronidazole is not recommended for pregnant women; although not absorbed and not highly effective, paromomycin may be used to treat giardiasis in pregnancy. Tinidazole has also been used and has been proven more effective than metronidazole as a single dose. Furazolidone is another option, but has been reported to be mutagenic and carcinogenic.
In the absence of a parasitologic diagnosis, the treatment of suspected giardiasis is a common question with no clear-cut answer. The approach depends on the alternatives and the degree of suspicion of giardiasis, both of which will vary among patients and physicians. However, it is not recommended that treatment be given without a good parasitologic workup, particularly since relief of symptoms does not allow a retrospective diagnosis of giardiasis; the most commonly used drug, metronidazole, targets other organisms besides G. lamblia.
The third question involves treatment of a patient who is asymptomatic. Generally, it is recommended that all cases of proven giardiasis be treated because the infection may cause subclinical malabsorption, symptoms are often periodic and may appear later, and a carrier is a potential source of infection for others. Certainly in areas of the world where infection rates, as well as the prospect of reinfection, are extremely high, the benefit-per-cost ratio would also have to be examined.


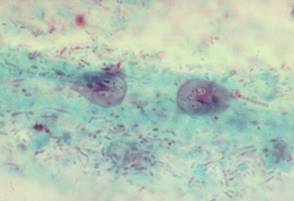
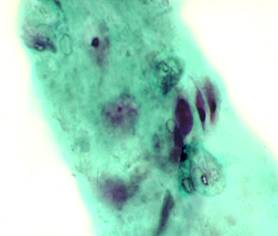

Three images of Giardia lamblia from positive stool specimens (from left to right: cyst seen in wet preparation from fecal concentration; trichrome permanent stain showing trophozoite; (lower) trichrome stain showing trophozoites in mucus; scanning EM of trophozoite attached to the gut lining. Note the internal details are somewhat difficult to see in the cyst (wet preparation, high dry examination), while the trophozoite morphology is more clearly seen on the trichrome stain, oil immersion examination).
REFERENCES:
Garcia, LS, 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, DC.
Garcia, L.S. 2009. Practical Guide to Diagnostic Parasitology, 2nd Ed., ASM Press, Washington, D.C.
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.