

***Reminder: Slides are copyrighted and cannot be copied for publication.
A 44 year old male was admitted to the hospital with complaints of severe diarrhea that had become worse over an extended period of weeks. This patient had previously been diagnosed as having AIDS and had been receiving HAART (highly active anti-retroviral therapy) for several years. Unfortunately, resistance to protease inhibitors in this patient was followed by a decrease in CD4 count and an increase in viral load.
He was treated with supportive care, and various specimens were submitted for diagnostic testing. Based on the images below, can you suggest the diagnosis? What organisms tend to match the image?

Left image: Wheatley's trichrome on stool (organisms 4-6 microns); right image: modified acid-fast stain (using a 1% acid decolorizer) (organisms 4-6 microns)
Based on this finding, additional testing was performed (modified trichrome stains) and the following images were seen.
(Left) Ryan-Blue modified trichrome; (Center) Ryan-Blue modified trichrome (urine sediment); (Right) combination modified acid-fast/modified trichrome stain; all photographed using oil immersion (x1000).
What organisms might be present in these images shown above?
(Scroll Down for Answers and Discussion)
ANSWER AND DISCUSSION OF DIAGNOSTIC QUIZ #54
The images presented in Diagnostic Quiz #54 are the following:
Images:
Top Row
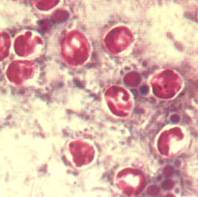
Left image: Cryptosporidium spp. oocysts stained using the Wheatley's trichrome stain on stool. Since the oocysts do not stain using this routine Ova and Parasite stain, they appear as clear objects on the permanent stained slide.
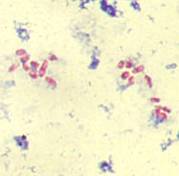
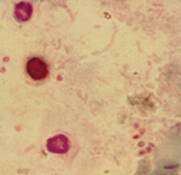
Right image: Cryptosporidium spp. oocysts stained using the modified acid-fast stain and a 1% acid decolorizer. Additional studies were performed and the following images were seen. Note that the sporozoites can be seen within some of the oocysts. Cryptosporidium oocysts are immediately infectious when the stool is passed, regardless of the stool consistency (liquid, formed).
Bottom Row
Left image: Microsporidian spores (stool specimen) stained with the Ryan-Blue modified trichrome stain. Note the pink spores. It is highly likely that microsporidian spores are immediately infectious when the stool is passed.
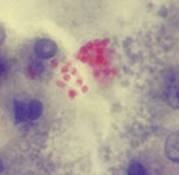
Center image: Microsporidian spores (urine sediment) stained with the Ryan-Blue modified trichrome stain. Note the pink spores. Because these infections often disseminate from the GI tract to the kidneys (and other body sites), urine, as well as stool, is usually examined as well.
Right image: Cryptosporidium spp. oocysts and microsporidian spores stained with a combination modified acid-fast and modified trichrome stain. Approximately 30% of patients with cryptosporidiosis also have microsporidiosis.
Comments on the Patient:
This case represents a dual infection with Cryptosporidium spp.and microsporidia in an AIDS patient who has developed resistance to HAART. The introduction of HAART has resulted in a significant decrease in HIV and AIDS-related mortality and morbidity. However, these treatments can select for drug-resistant viruses that are associated with poor responses to the antiretroviral therapy and possible loss of clinical benefit. Unfortunately as a decrease in CD4 count and an increase in viral load were seen, the patient also developed diarrhea caused by both Cryptosporidium spp. and microsporidia. In a compromised patient, the diarrhea can be quite severe and prolonged, with tremendous fluid loss and eventual death. With the advent of the use of Highly Active Antiretroviral Therapy (HAART) (from 1996 on), there has been a significant reduction in the incidence of cryptosporidiosis. Unfortunately, this patient had developed resistance to the therapy. With increased resistance being seen in more AIDS patients, cases of symptomatic cryptosporidiosis and microsporidiosis may become more common as they were in the early 1990's.
Comments on the Organisms:
Currently, Cryptosporidium hominis is thought to infect humans, while C. parvum can infect various mammals, including humans. Cryptosporidium spp. is worldwide in distribution, and although the first cases in the literature indicated the patients were immunosuppressed or immunodeficient, much of the published literature reports infections in patients with a normal immune capability. In patients with a normal immune capability, cryptosporidiosis is self-limiting. However, in certain compromised patients, the diarrhea can be very severe and prolonged, with eventual death as the outcome. Clinical symptoms include nausea, low-grade fever, abdominal cramps, anorexia, and 5 to 10 watery stools per day. Fluid loss in these patients is significant and has been reported to be as great as 17 liters/day. Although many therapeutic regimens have been tried, there is no completely satisfactory therapy for cryptosporidiosis in humans. Respiratory cryptosporidiosis has also been reported in AIDS patients. Sputum specimens should be submitted in 10% formalin or as a fresh specimen and can be examined by using the same techniques as used for stool samples.
CRYPTOSPORIDIUM KEY POINTS - LABORATORY DIAGNOSIS
1. If the specimen represents the typically watery diarrhea, there should be numerous organisms that may be caught up in mucus.
2. The more normal the stool (semiformed, formed), the fewer the organisms and the more artifact material that will be present.
3. Several concentrates and at least five or six modified acid-fast smears should be examined before a patient is considered negative, especially if the patient has been on experimental medications.
4. The normal permanent stains (trichrome, iron hematoxylin) do not adequately stain Cryptosporidium spp., although occasionally oocysts may be seen in these preparations, especially in heavy infections.
5. Although the organisms can be stained with auramine-rhodamine stains, they should be confirmed by using acid-fast stains or the monoclonal reagents (most sensitive). This is particularly true if the stool contains other cells or a lot of artifact material (more normal stool consistency).
6. Sputum specimens should be submitted in 5 or 10% formalin and processed in the same way as a stool sample.
7. It is important to remember that in severely immunocompromised patients <100 CD4+ cells), microsporidia may also be present in approximately 30% of those patients who have cryptosporidiosis. The diagnostic procedures for the identification of Cryptosporidium spp. will not be appropriate for the identification of microsporidial spores. Modified trichrome stains and optical brightening agents (Calcofluor white) can be used for that purpose.
The microsporidia are obligate intracellular parasites that have been recognized in a variety of animals, particularly invertebrates; the organisms found in humans tend to be quite small, ranging from 1.5 to 2 microns. Until recently, awareness and understanding of human infections have been marginal; only with increased understanding of AIDS within the immunosuppressed population has attention been focused on these organisms. Limited availability of EM capability has also played a role in our inability to recognize and diagnose these infections. Current genera include: Anncaliia, Brachiola, Encephalitozoon, Septata, Enterocytozoon, Microsporidium, Nosema spp., Pleistophora, Trachipleistophora, and Vittaforma.
A number of cases of infection with Enterocytozoon bieneusi and/or Encephalitozoon (Septata) intestinalis have been reported in AIDS patients. Chronic intractable diarrhea, fever, malaise, and weight loss are symptoms with E. bieneusi infections, symptoms that are similar to those seen with cryptosporidiosis or isosporiasis. These patients have already been diagnosed with AIDS and each day tend to have four to eight watery, nonbloody stools which can be accompanied by nausea and anorexia. There may be dehydration with mild hypokalemia and hypomagnesia, as well as d-xylose and fat malabsorption. The patients tend to be severely immunodeficient, with a CD4 count always below 200 and often below 100. E. bieneusi infection has also been implicated in AIDS-related sclerosing cholangitis. Dissemination to kidneys, lower airways and biliary tract appears to occur via infected macrophages. Infections with E. intestinalis tend to respond to therapy with albendazole, unlike the infections with E. bieneusi.
E. bieneusi spores have been identified in the sputum and bronchoalveolar lavage, as well as stool samples, from a patient with a 2-year history of intestinal microsporidiosis. Although no pulmonary pathology could be established in this or one other reported case, it is well established that E. bieneusi is capable of colonizing the respiratory tract and these clinical specimens may reveal the presence of spores. Using transmission electron microscopy, multiorgan microsporidiosis due to E. bieneusi has been diagnosed in an HIV-infected patient; organisms were recovered in stools, duodenal biopsy, nasal discharge, and sputum. Infection with this organism has also been reported in individuals with intact immune function; symptoms were self-limited and diarrheal disease resolved within 2 weeks; a number of other cases have been reported in immunocompetent people. These cases suggest that E. bieneusi may be more commonly associated with sporadic diarrheal disease than was suspected and that the immune system may play a role in the control of this organism within the intestine.
MICROSPORIDIA KEY POINTS--LABORATORY DIAGNOSIS
1. It appears from the literature that approximately 30% of AIDS patients and those with cryptosporidiosis may also have infections with microsporidia. In this group of patients with chronic diarrhea, microsporidian infections must be considered.
2. The modified trichrome staining procedure for stool may be difficult to interpret without positive controls to review. Make sure that the material on the slides is very thin, the smear is stained for the recommended time frame, and the smear is examined under oil immersion (total magnification of at least x 1,000).
3. The optical brightening agents (Calcofluor, Fungi-Fluor, and Uvitex 2B) provide a sensitive screening method, but the results are nonspecific. False positives have been reported due to fluorescent artifact material.
4. As monoclonal or polyclonal antibody reagents become commercially available, we may see diagnostic procedures with greater specificity and sensitivity. Reagents are currently being used in a few institutions; these preparations are generally easier to read than are the routine stains.
5. Touch preparations can be methanol fixed and stained with Giemsa.
6. Plastic-embedded tissues stained with PAS, silver, acid-fast, and routine hematoxylin-eosin stains generally stain better than paraffin-embedded tissues. This finding may be related to the use of formalin as a tissue fixative.
7. Be sure to gain some experience in examining these preparations before sending out patient specimen results. This work almost mandates the use of positive control material, regardless of which technique(s) is used. Once a laboratory has gained experience with these methods, it is appropriate to begin accepting clinical specimens.
8. EM is the ``gold standard'' for confirming infection and for attempting to classify the organisms seen in tissues. However, EM procedures may not be as sensitive as some of the other available methods.
9. It is recommended that more than one procedure be used when working with stool specimens (modified trichrome, optical brightening agent); this is primarily because of the high number of artifacts present in stool. Urine and other body fluid specimens are much easier to examine for the presence of microsporidial spores.
REFERENCES
Garcia, LS, 2016. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, DC.
Garcia, L.S., R.Y. Shimizu, and D.A. Bruckner. 1994. Detection of Microsporidial Spores in Fecal Specimens from Patients Diagnosed with Cryptosporidiosis. J. Clin. Microbiol. 32:1739-1741.
Ives, N.J., B.G. Gazzard, and P.J. Easterbrook. 2001. The changing pattern of AIDS-defining illnesses with the introduction of highly active antiretroviral therapy (HAART in a London clinic. J. Infect. 42:134-9.
Vaclavikova, J. et al. 2005. Long-term analysis of the resistance development in HIV-1 positive patients treated with protease and reverse transcriptase inhibitors: correlation of the genotype and disease progression. Acta Virol 49:29-36
Wittner, M. and L.M. Weiss (eds). 1999. The Microsporidia and Microsporidiosis. ASM Press, Washington, D.C.
Each Quiz has a two section format: the first section will present the Quiz topic and the second section will provide a discussion of the answer and/or various options in response to the Quiz situation presented to the user. In some situations, there may be more than one correct response.
The content within this site is made possible through the extensive contribution of Lynne S. Garcia, M.S., MT(ASCP), CLS(NCA), BLM(AAB), F(AAM), Director, Consultantation and Training Services (Diagnostic Medical Parasitology and Health Care Administration). For additional information, she can be contacted at LynneGarcia2@verizon.net.
Reference: Garcia, L.S. 2015. Diagnostic Medical Parasitology, 6th Ed., ASM Press, Washington, D.C.